I'm new here!
Hi, my name is jenpanky. I'm here because
Hi, my name is jenpanky. I'm here because
Hi, my name is Deevine1973. I'm here because these are my diagnoses, but they don’t have me!
#MightyTogether #Anxiety #Depression #BipolarDisorder #BorderlinePersonalityDisorder #Fibromyalgia #ADHD #PTSD #RheumatoidArthritis #EatingDisorder #AutoimmuneHyperlipidemia #AutoimmuneThyroidDisease #AutoimmuneRetinopathy #AutoimmunePancreatitis #LupusNephritis #ChronicPain #ChronicKidneyDisease #ChronicPancreatitis #ChronicFatigueSyndrome

Just joined “The Mighty” today. I have Multiple Sclerosis, Chronic Pancreatitis (With chronic pain) and diabetes secondary to chronic pancreatitis. (And a host of other diagnoses… but those are the big ones. I am a medically retired nurse. I struggle with chronic pain, fatigue, muscle spasms, nutritional deficiency, migraines. Not being able to work has really impacted our financial stability and my sense of self esteem. I fight loneliness and isolation. My husband works 50+ hours a week (As he is our source of medical insurance and primary “Bread winner”). I have 2 adult sons who have their careers and social life. All our family is out of state. I hope to connect with other people who know what living with chronic illnesses is like. I also look forward to others pearls of wisdom. # multiple sclerosis #chronic pancreatitis #Diabetes #chronic pain #Fatigue
Hi, my name is Sunflowers4Susan. I'm here because I have multiple incurable diseases. I find that my illness have progressively isolated me, and I miss people and my career terribly. I am looking for people who can identify and share how living with chronic illness changes us. I would like to find inspiration and strength from others. I am longing for hope in the face of fear. I am searching for some grace in the gray.
#MightyTogether #MultipleSclerosis #Migraine #PTSD #ChronicPancreatitis #Diabetes
Hi, my name is Sandeepjain1805. I'm here because I have been ill all my life - diagnosed with Chronic Pancreatitis at the age of 7, I am today left with no pancreatic function. My glands have weakened considerably. And now I have been diagnosed with neurogenic bladder and prostatitis. My anxiety levels are usually high. Mostly bedridden now, I am looking deep within to help get out of this....
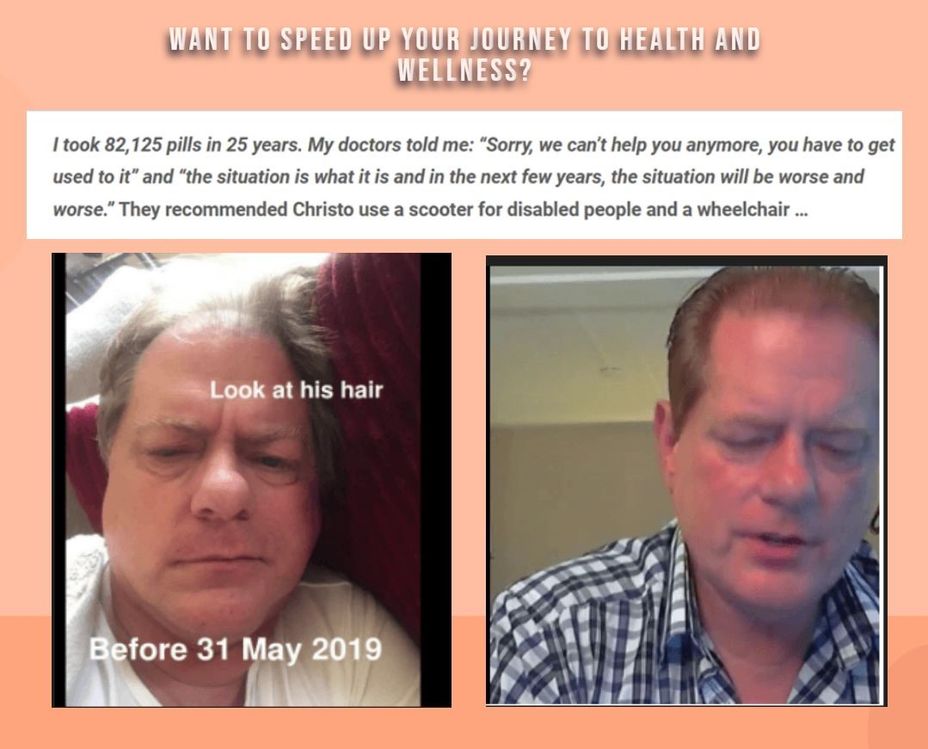
Meet Kristo—he suffered from pains in his body, fibromyalgia, three heart attacks, and one stroke, and has been using a sleep apnea device since 2012.
After 25 years of diligently following the medications and surgeries prescribed to him, his long-term doctors informed him in mid-May 2019 that they could no longer do anything for him. By this point, his body had deteriorated significantly.
He could no longer walk well. His vision was only 30% after two failed eye operations. Using two crutches, he could move a maximum of 100 meters before losing balance and falling over due to the pain. He had been suffering from chronic fatigue for at least 30 years, dragging himself through each day.
His wife, his caregiver for many years, juggled her job in childcare with an unpaid "job" as a nurse, driver, cook, cleaning lady, gardener, and chef, leaving her little time in her busy, hectic life.
Kristo was told to get comfortable in a scooter for disabled people and a wheelchair because that was going to be his life going forward. Their world fell apart - until a friend introduced him to our program.
See the new man! Kristo’s journey from chronic fatigue and debilitating pain to renewed vitality is just one example of how our program is helping many people get their lives back holistically, without medications and surgeries.
We are looking to talk to 60 men and women, especially those over 50, who have health problems and are serious about finding a proper solution.
Your insights will help us build a program tailored to your needs. Participants will be rewarded with a 10% discount when the program launches. It provides transformative results, by the way.
Interested? YES or NO?
Comment below if you want to participate!
Thanks!
#ChronicFatigue #ChronicIllness #ChronicDailyHeadache #ChronicLungDisease #ChronicPain #chronic #ChronicLungDisease #ChronicInflammatoryResponseSyndrome #ChronicPancreatitis #ChronicTraumaticEncephalopathy #ChronicObstructivePulmonaryDisease #ChronicOrthostaticIntolerance #ChronicVestibularMigraine #MentalHealth #Addiction #chronic #Anxiety #Arthritis #BackPain #CeliacDisease #CommonVariableImmuneDeficiency #ComplexRegionalPainSyndrome #Eczema #EosinophilicEsophagitis #HashimotosThyroiditis #ChronicLymphocyticLeukemia #HashimotosThyroiditis #InflammatoryBowelDiseaseIBD #InterstitialCystitis #IrritableBowelSyndromeIBS
Hi everyone, my name is Kyle and I’m new to this app. I was just curious if anyone in this group has chronic pancreatitis. I was in the hospital last spring for 2 months with a 50/50 chance I was going to make it . I’m hoping to chat with anyone with this illness and get some advice on how to deal with pain and the constant discomfort.
Hey , my name is Kyle and I’m new to this . I was in the hospital for 2 months last spring with a 50/50 chance of making it out . I have chronic pancreatitis, and I was just wondering if anyone else on here has that same chronic illness . If so could you reach out , certainly be nice to find others and talk about how they deal with this constant discomfort and pain . 🍻
Hi, my name is NGlucina111. I'm here because I have chronic necrotizing pancreatitis,inertia hernia in my groin ( which honestly is almost more painful than CP) one kidney and a decent variety of other issues!!
Hi, my name is Norasusan. I'm looking for