As a recently diagnosed person with Sjögren’s Syndrome, Undifferentiated Connective Tissue Disorder, Hydradenitis Suppurativa, POTS, and Ehlers Danlos syndrome, I am coping and learning.
My journey started in May of 2022, when I complained to my PCP that my dermatologist kept telling me that my hives were a problem for my allergist, but my allergist kept claiming they didn’t do anything with those, to talk to dermatology.
She asked about any other symptoms, knowing I already had a history of ADHD, anxiety, PCOS, uterine fibroids, endometriosis and GERD. She asked about pain and I told her I always have some pain, but it’s never anything major and never consistently placed in my body. She asked about headaches and migraines, energy levels, dizziness, fatigue, about stomach issues and my bowel and bladder frequencies. She asked about my family history. She decided to run a multitude of labs including a THS, CBC, CMP, and ANA. When the ANA came back positive, she said we’d found an answer. Well, not the final answer, but we’d found a direction. So off to the rheumatologist I went.
After one very dismissive rheumatologist 3 months later, I found another rheumatologist 2 hours away that was recommended by a friend. This doctor accepted the tests that were previously ran by my PCP, added more tests to my list including another ANA and AVISE testing. This was how we determined what I had.
Originally thought to be lupus, (It’s never lupus!- House) they found Sjögren’s Syndrome primary, with UCTD in there as well. The UCTD could eventually become LUPUS, but I didn’t meet the full markers for a lupus diagnosis. With this diagnosis, I did the base line eye exams and began taking Plaquenil. While taking this, I still experienced pain, motility issues, and other things but after 6 months, I could definitely feel a significant reduction in my pain, fatigue, and brain fog. This alleviated a significant portion of my pain, which in turn reduced my anxiety and depression. On top of this, I also read about joint health and increased my Vitamin D intake (which had always been low without a supplement) and added Glucosamine, Turmeric, Ginger and Black Pepper supplements to help with any nutritional deficiencies. Since I have continued to decline every time my body encounters a virus, I have increased my water intake, reduced my caffeine and sugar intake, and made some major lifestyle changes.
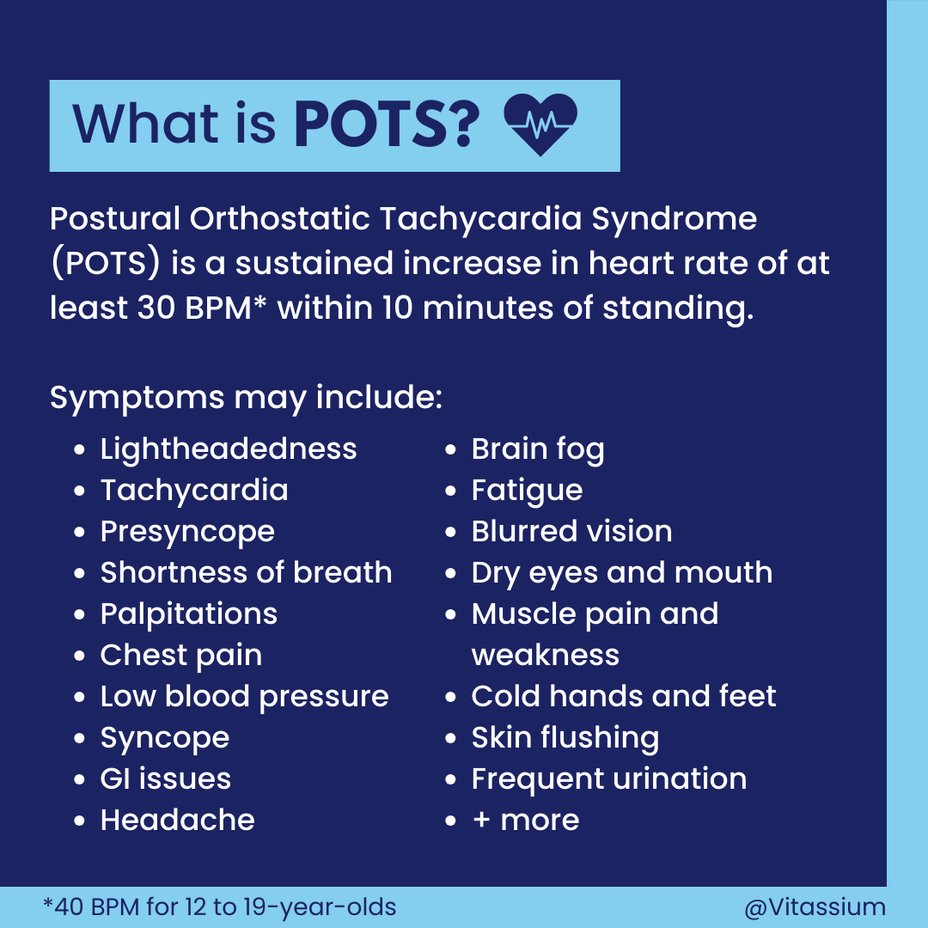
Among my lifestyle changes, I have been advised by my rheumatologist to avoid the Sun. I’m naturally fair skinned so I already wore sunscreen but he told me that this goes beyond that. To cover my skin, wear a hat, sunglasses, and try to avoid being out in direct sunlight as much as possible. I have also learned that my excessive sweating is not just me being out of shape, but that my body fails to properly regulate my body temperature. It is a part of my disautonomia. Getting that diagnosis led to a cardiology work up, which indicates my life long fainting issues are POTS and nuerocardiogenic syncope, not “low blood sugar” as I’d always been told. I am currently awaiting an echo stress test to determine the cause of my exercise intolerance which has kept me out of the gym for 2 years. Basically, when my heart rate gets above 100 I start to sweat profusely. At 130, I get dizzy and lightheaded. At 140-150, I begin to see spots and my vision blurs and I have to sit down before I faint. I used to go to the gym and do the BodyPump, Zumba and cardio kickboxing classes 3-4 times a week, but I haven’t been able to make it through a whole class in 2 years. (Thanks COVID!)
I’m March of 2023, I finally decided to go back to the dermatologist (albeit a different company than before) to have them help me with my skin issues like cystic acne and spots that just wouldn’t heal under my arms and around my breasts. After doing more research and talking with an RN whose sister has HS, the dermatologist and I agreed that I do in fact have HS, not just cystic acne. We treated with a round of antibiotics and steroids, which made a difference temporarily. The other option she recommended is for Humira, but that is a much stronger treatment option. We decided to go the easy route currently, since Humira is not covered by my insurance.
Upon getting yet another virus in July, I became even more pained, resulting in my near trip to the emergency room due to 8 out 10 pain that I could not pinpoint in my body. My PCP thankfully worked me in, and gave me a steroid and antibiotic shot in office, plus sent me in a medrol pack and augmentin to help. She said if my pain didn’t reduce by the next day, to go to the emergency room. She ran more labs, which showed my calcium was high, so she sent me in for a thyroid echocardiogram which should no abnormalities. My doctors have all suspected thyroid issues for years, but I’m always within normal range, but on the low end.
We managed to get my pain under control, but I still have wounds that won’t heal, pain I can’t explain and more fatigue. I’m currently going to physical therapy because at that July appointment, she diagnosed me with EDS. Physical therapy helped me get my pain under control and I no longer wake up in pain. I’ve learned a lot of new exercises that do not stress my heart but strengthen my core, and loosen my muscles without stretching my joints. I’ve learned how to adjust my posture and added a seat cushion to my car, since that is where I am most of the day. I’ve learned why I just want to lay down when I’m hurting or feeling exhausted. My blood pressure is struggling to regulate itself, and I feel faint and lightheaded upon standing or while standing for too long.
I’ve also learned why my depression gets so bad. Who knew inflammation can cause severe, mind altering depression? I’ve struggled for years with intrusive thoughts but I knew I wasn’t typically depressed because I never considered suicide. I simply could tell my brain wasn’t working right, but I had no clue why.
Ugh, this has been a rambling mess, but it’s the simplest way to explain everything that has changed about me this year. And it’s a lot. I know I’m nowhere near through learning, but I hope to find the right answers. I’m reading about diet and looking for a job that still pays well but allows me to avoid the Sun, so maybe something WFH? Who knows what I’ll look like or life will be like next year, but I’m thankful for the answers I have and the answers to come. If you relate to any of these, please feel free to comment. It’s nice to know you’re not alone in all this.
#EhlersDanlosSyndrome #SjogrensSyndrome #UndifferentiatedConnectiveTissueDisease #HidradenitisSuppurativa #POTS #Dysautonomia #NeurocardiogenicSyncope