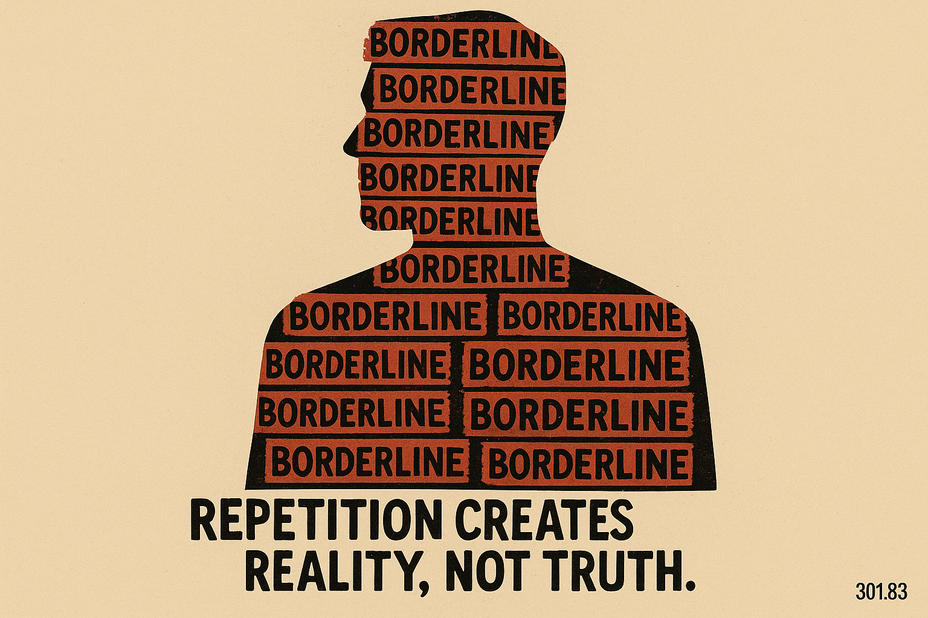
I discovered a label in the margins of a chart and watched gravity shift. Arguments began reading as “affect.” Risk assessments read as “instability.” Safety calls arrived preloaded with suspicion. The file learned a new word; the room learned a new posture.
Here is the claim: the BPD label often operates as an administrative alias for trauma. First, testimony loses credit. Then isolation sets in. Protest finally appears as “symptom.” Philosophers call the first move epistemic injustice and the aftermath ethical loneliness. Clinicians call the visible residue “borderline.” The engine underneath runs on trauma physiology, attachment disruption, and the long tail of disbelief.
Checklists describe; histories explain. The DSM clusters collapse neatly into trauma signatures:
Affect storms track hypervigilance and arousal cycles; anger acts as perimeter when safety feels provisional.
Relational whiplash follows nervous systems trained to anticipate loss; closeness alarms, distance invites pursuit.
Self-state wobble and dissociation reflect survival’s constant self-editing under threat.
Short-horizon choices (branded “impulsivity”) often function as rational relief under scarcity and uncertainty.
This trajectory has a public health shape: credibility discounts → isolation → protest behaviours that read as essence. The behaviours look dramatic; the mechanism reads simple. Harm without uptake teaches escalation. People intensify when unheard, conserve when ignored, and scan when help proves conditional.
Care systems stabilize categories across sites—intake, unit, record—because categories move paperwork. Labels travel fast; justice travels truer. Precision in formulation matters because it governs what gets treated: character or injury.
Choose a different architecture:
Lead with trauma-grounded, function-based formulations (PTSD/CPTSD where it fits).
Practice epistemic justice out loud: name uptake, audit disbelief.
Build plans that reduce arousal, widen windows of tolerance, and keep police out of care loops.
Chart triggers, functions, and levers; retire global character verdicts.
read the original blog post where i go into the details of this theory here ----> Borderline Personality Disorder (BPD): A Fake Disease They M... #BPD #BorderlinePersonalityDisorder #Trauma