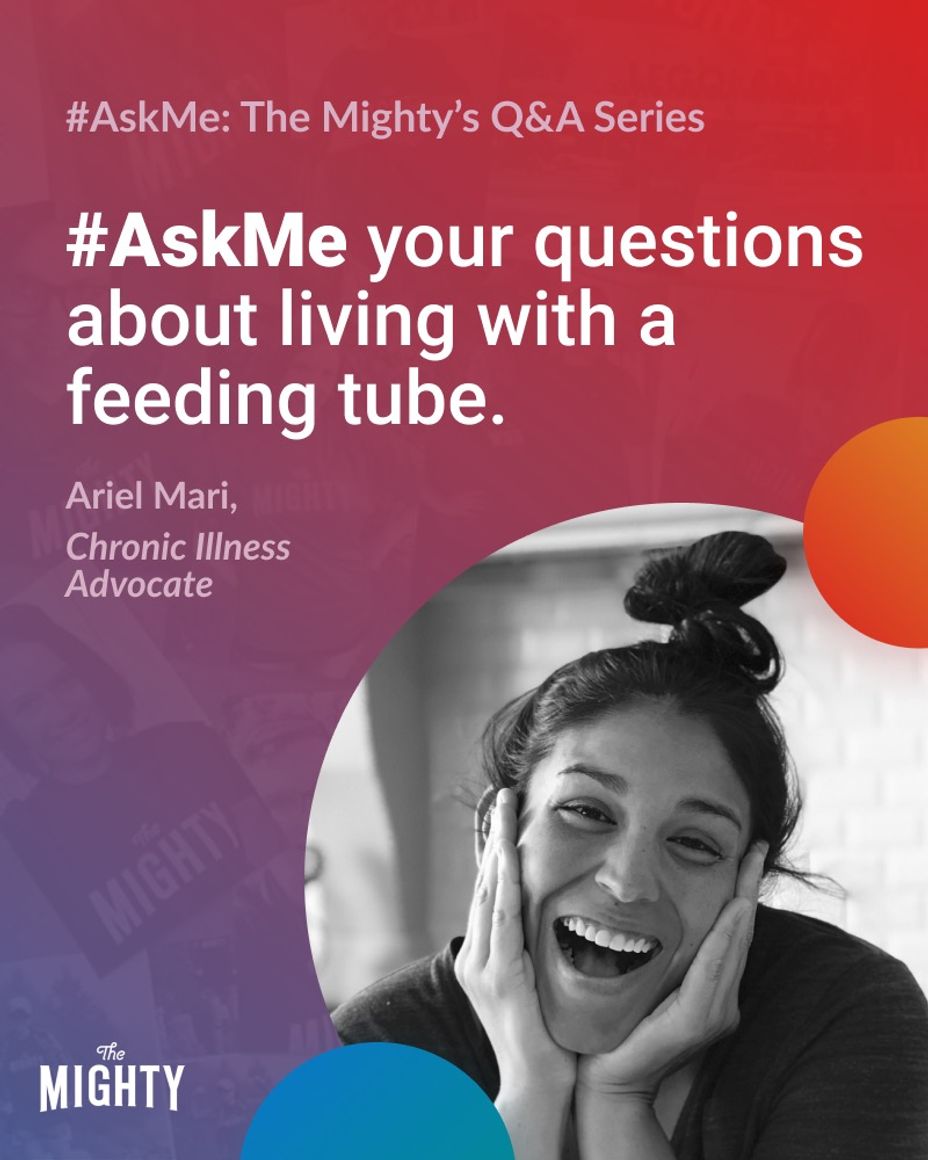
#FeedingTube #ChronicIllness #Gastroparesis #Spoonie #FeedingTubes
Hi Mighties!
My name is Ariel and I am a chronic illness advocate and have lived with gastroparesis for the last 6 years and 2 of those years with a feeding tube. During this week I’ll be answering questions about life with a feeding tube and some tips and tricks I have picked up that have been beneficial in my day to day life with a feeding tube.
[Note: I am not a medical professional and cannot dispense medical advice of any nature.]
I look forward to answering your questions. You can post them in the comments below and I will answer them throughout the week!