Hi, my name is cdeevers. Hi, I’m Carolyn! I’m a writer, memoirist, and longtime advocate for people navigating hard things—chronic illness, trauma, and complicated relationships.
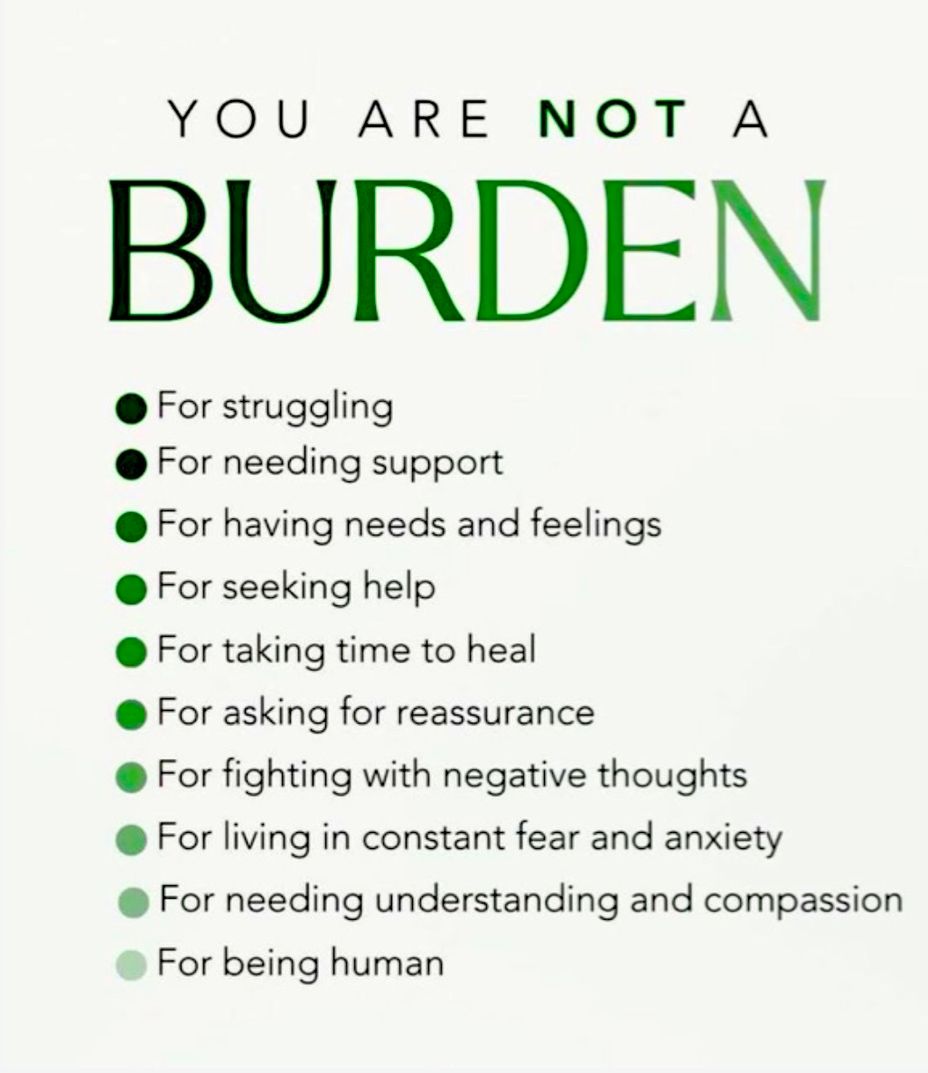
My own health journey has been anything but straightforward. After decades of misdiagnoses, I finally began piecing together answers about my conditions and how they connected to prolonged stress and trauma. Those experiences shaped not just my health, but also my writing.
I write personal essays, a blog, memoirs, and articles about resilience, faith, and the hidden costs of living through crisis—like my book-in-progress, Knock Knock, Neighbor Tales. My work combines raw honesty, a dash of humor, and a deep belief that our stories can help others feel less alone.
If you’ve ever felt unseen in your health journey or overwhelmed by what life has thrown at you, you’re in the right place. I’d love to connect, share, and learn from one another here.
#MightyTogether #PTSD #LymeDisease #NeuropathyHereditary #MastCellActivationDisorder