#Insomnia #CBT
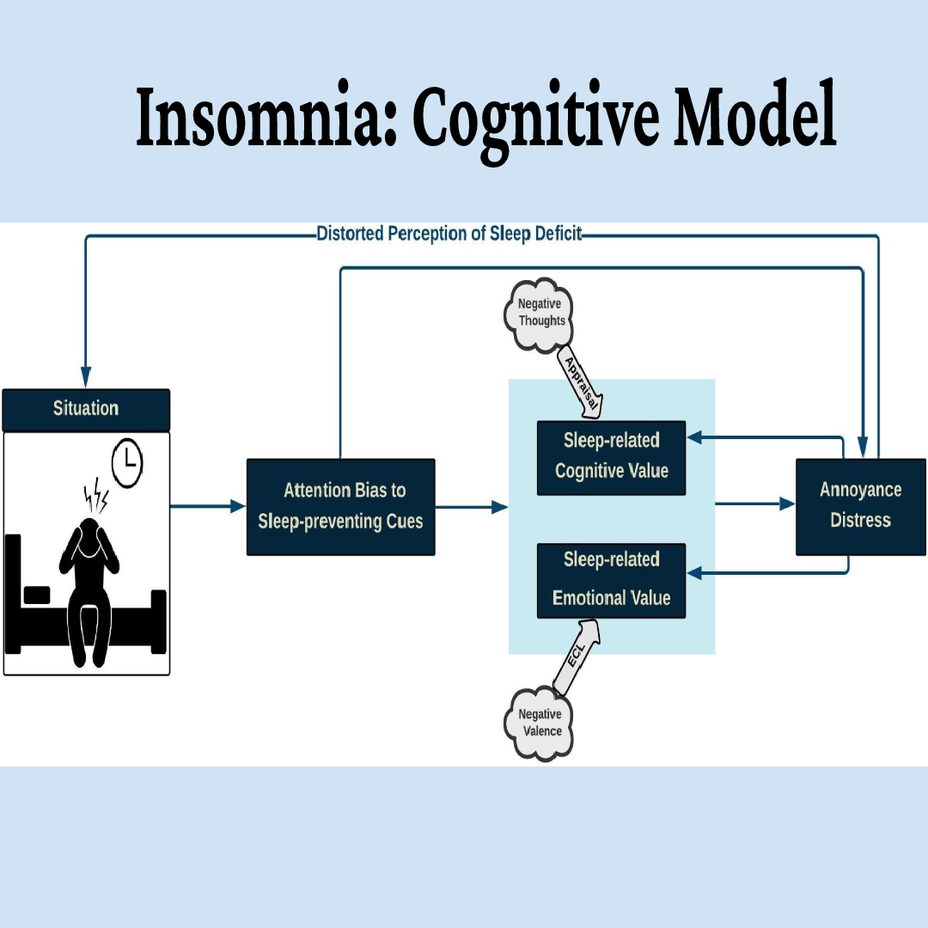
Situation
Nighttime silence in the pre-sleep period can facilitate CAAP of internal (body sensation or thoughts) and external (environmental sounds, light, and heat) stimuli. Bootzin and Rider (1997) noted that “bedtime may often be the first quiet time during the day available to think about the day’s events and to worry and plan for the next day.” Therefore, bed and bedtime tend to be cues for arousal rather than for sleep.
Attention Bias
Consciously attended internal and external stimuli develop an individual’s predictions and expectations from the pre-sleep situation. One of the commonly used paradigms for experimental assessment of attentional bias is the Dot-Probe task. In this, a pair of stimuli (e.g., words or pictures) are presented simultaneously at different locations (up/down or top/bottom) on the screen.
The stimuli pair disappear after a fixed time window and a probe appears in the location of emotional (congruent presentations) or neutral (incongruent presentations) stimuli. Subjects are asked to detect and respond to the location of the probe as fast as possible, and the attentional bias is measured through their reaction time in responding to the probe location.
Most of these studies have endorsed the notion that poor sleepers display attentional bias to sleep-related cues compared with controls. Jansson-Fröjmark et al. (2012) used a dot-probe task to demonstrate that individuals with primary insomnia had a considerably prolonged reaction-time when shifting attention away from insomnia-associated pictures paired with neutral pictures, in comparison to neutral-neutral paired picture presentations as control.
Emotional Value
The emotional value gets shaped through the evaluative conditional learning (ECL) mechanism which plays a crucial role in liking and disliking stimuli (Ghodratitoostani et al., 2016a, b). Based on ECL, neutral stimuli (CS) can obtain either positive or negative valence after being repeatedly paired with emotion-laden stimuli (US) (De Houwer et al., 2001). Valence represents emotional states varying along a spectrum, ranging from positive to negative feelings with a neutral center-point (Bradley and Lang, 1994). Based on the CCF, CAAP of both CS and US, and their contingencies are required at the time of EC-learning formation.
Additionally, evaluative conditioning is an accumulative procedure through which different valenced USs can add to CS valence after being repeatedly paired (Stahl and Unkelbach, 2009). Therefore, EC-learning is resistant to extinction so that neither individual CS/US presence alone, nor pairing CS with different USs would cause the extinction of previously shaped evaluative conditioning (De Houwer et al., 2001).
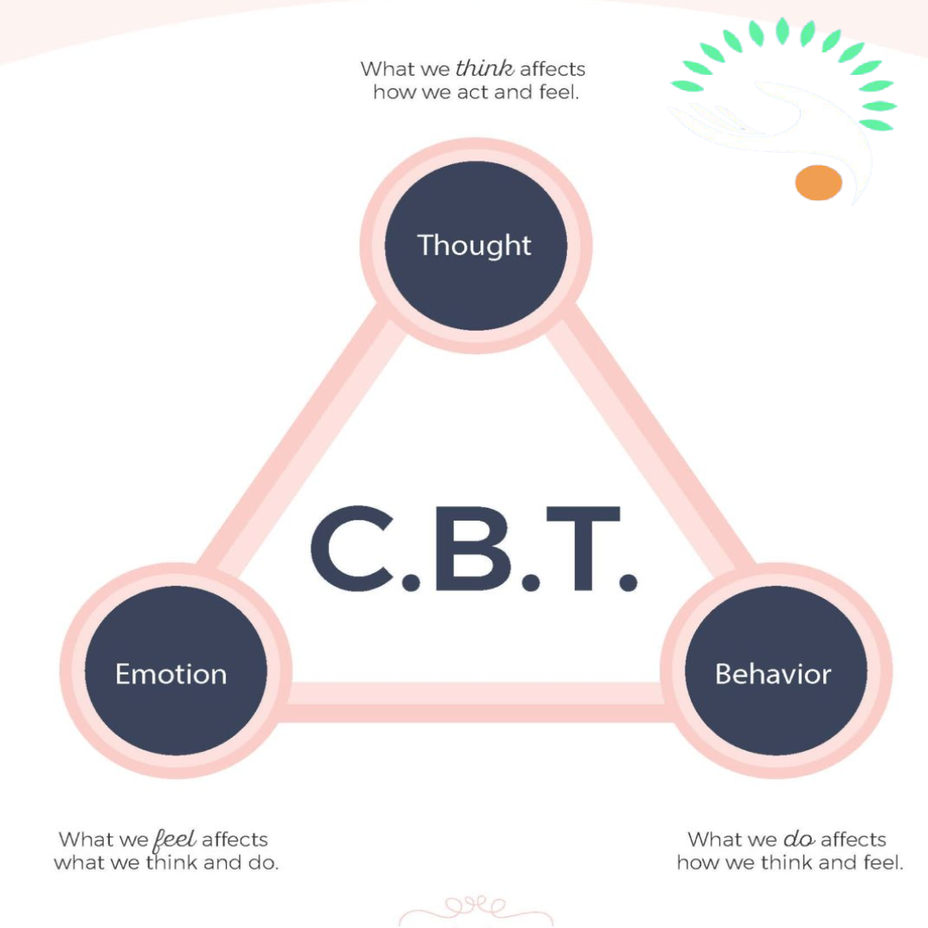
Cognitive Value
The cognitive value related to internal and external stimuli is built through an appraisal process. This process initiates when the meaning of an object or event is evaluated in a particular situation according to pre-existing beliefs, desires, and intentions (Scherer et al., 2001). However, not all information but that relevant to individuals’ concerns (Frijda, 1987), can trigger a cognitively aroused state followed by the appraisal.
Accordingly, attention bias to sleep-preventing cues (as concern-relevant stimuli) can trigger a cognitively aroused state with subsequent appraisals about insomnia, “I am never going to get to sleep,” “I am not coping with the amount of sleep I get,” and “I am going to lose my job” (Harvey, 2002). Negative thoughts through this appraisal mechanism further fuel the negative sleep-related cognitive value, leading to annoyance or distress reaction.
Annoyance-Distress Reaction
Consistent with many cognitive-behavioral studies, the CCF suggests that negative appraisals of insomnia trigger the annoyance-distress reactions. According to the cognitive model of insomnia, excessively negative thinking in the pre-sleep time provokes autonomic arousal, and emotional distress (Harvey, 2002). Tang and Harvey (2004a) have reported that the manipulation of psychological and physiological arousal produces adverse effects on the perception of sleep quality.
For illustrative purposes, Baglioni et al. (2010) presented five blocks showing neutral, negative, positive, sleep-related negative and sleep-related positive pictures to evaluate the psychophysiological reactivity to emotional stimuli, both related and unrelated to sleep, in people with primary insomnia and normal sleepers. facial electromyography, heart rate, and cardiac vagal tone were recorded during the picture presentation.
Distorted Perception
According to the CCF, valence and cognitive-arousal as two components of emotion can affect patients’ judgment about sleep quality perception. The following findings lend support to this proposal.
Yoo and Lee (2015) explored the effect of modulating arousal and valence on time-perception in subjects with social anxiety, comparing the time duration of the presented stimuli with the standard duration in training sessions. The perceived duration of negative-stimuli against positive-stimuli was longer with high arousal, but shorter with low arousal levels, suggesting that modifications in the type and magnitude of both valence and arousal modulate time-perception (Yoo and Lee, 2015). This may also be analogous to the distortion in sleep quality-perception in insomniacs.
You can refer to this:
resiliens.com/resilify/program/cognitive-behavioral-therapy-...